
Vaccinating the most vulnerable group in the time of pandemic: Insights from a national survey of older people
The University of the Philippines Population Institute (UPPI) in collaboration with the Demographic Research and Development Foundation (DRDF) are sharing results of their demographic studies to provide the Philippine context on the possible effects of the coronavirus disease (COVID-19) pandemic. In both the UPPI and DRDF websites, we are publishing a series of research briefs focusing on various aspects of Filipino lives that are affected by COVID-19, in both the short and long terms.
Download PDF here.
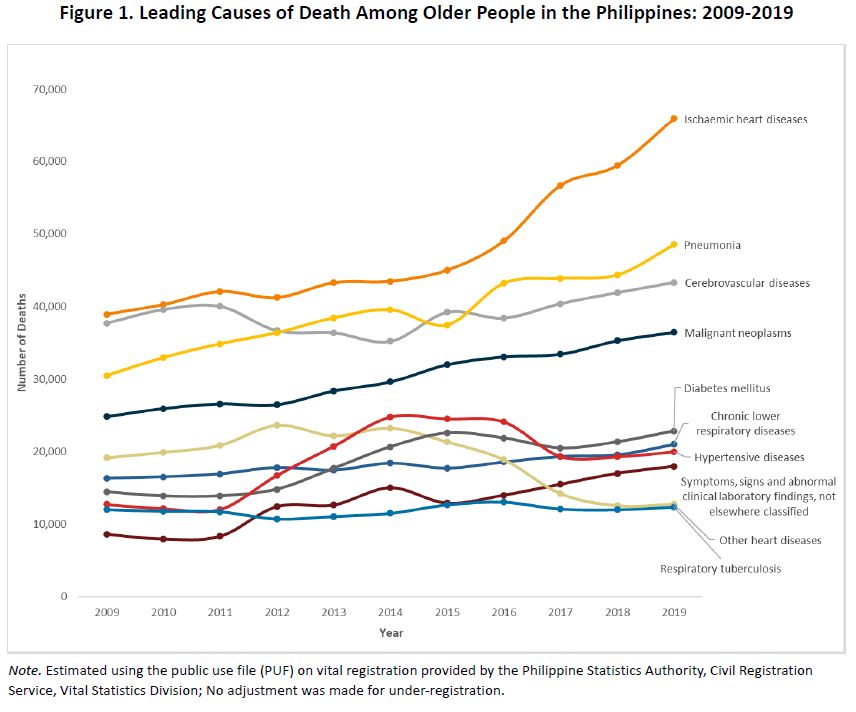
Influenza and pneumonia are two of the most common diseases among older people (OP) in the ages 60 years and over. In the Philippines, influenza was estimated to account for an average of 5,374 excess deaths per year or about 1.1% of the average annual all-cause deaths from 2009-2015. About 2 in 3 of these deaths occurred in adults 60 years old and over (Cheng, et al. 2020). Pneumonia, on the other hand, has been one of the leading causes of death among older Filipinos ages 60 years and over (see Figure 1). Accordingly, many international and local health societies including the Philippine Society of Microbiology and Infectious Diseases (PSMID) highly recommend persons aged 60 and older to be given the influenza and the pneumococcal vaccine to address these two important diseases: influenza and pneumonia (Berba, 2006).
In 2011, the Department of Health (DOH) launched free influenza and pneumococcal vaccination program for indigent older people (OP) in the country. Four years later, this vaccination program was expanded to cover all OP under the National Policy on Health and Wellness Program for Senior Citizens (HWPSC), which aims to prevent functional decline and disease in old age (DOH Administrative Order No. 2015-0009). Following the DOH’s implementing guidelines for the immunization of senior citizens, OP can avail of the recommended doses of pneumococcal polyvalent vaccine (an inactivated vaccine containing 23 killed pneumococcal strains) and influenza polyvalent vaccine (containing 3 killed influenza viruses) in public health care facilities (A. O. 2011-0018). Studies from other countries have shown that influenza or pneumonia vaccines are effective against acute symptoms of influenza and pneumonia infections (Heo, 2018; Kostova et al., 2013; Smetana, Chlibek, Shaw, Spino, Prymula, 2018). Since its rollout, however, no study had looked at the extent to which older Filipinos were covered by the vaccination program.
This research brief examines the Filipino older people’s awareness of influenza (more commonly called flu) and pneumococcal vaccines, their level of vaccination, and the extent to which these vary across selected characteristics of older people. The analysis is based on the data of the Longitudinal Study of Ageing and Health in the Philippines (LSAHP) 1 baseline survey, a nationally representative survey on older Filipinos ages 60 years and over conducted in 2018. The survey of 5,985 respondents included questions on whether OP are aware of flu and/or pneumococcal vaccines for older people, and if so, whether they have availed of these vaccines.
Awareness of flu/pneumococcal vaccines
Results show a low level of awareness of either of the two vaccines: only 3 in 10 are aware of the flu vaccine for older people while 4 in 10 are aware of pneumococcal vaccine. Flu and pneumococcal vaccine awareness are more common among older females, those in the younger age group, better educated, urban residents and those who belong to the higher socioeconomic groups.
Vaccine awareness does not translate to inoculation
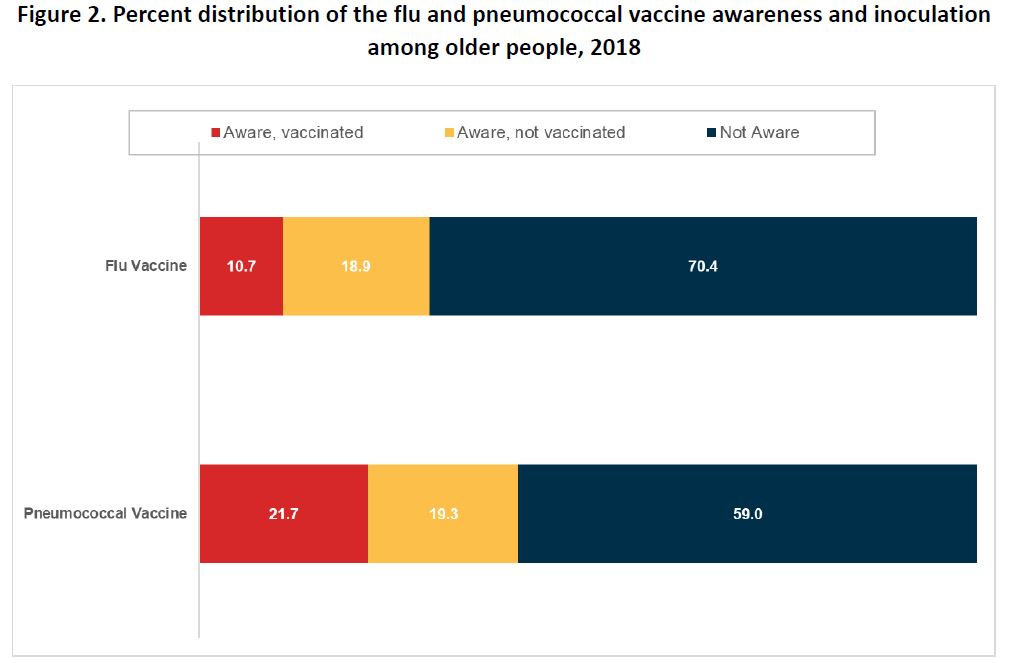
In addition to the low-level awareness of vaccines for older people, there is also a low percentage of OP who have been inoculated with either flu or pneumococcal vaccines. Among those who said they are aware of the flu vaccine for example, only 36% had been vaccinated against influenza since they reached the age of 60. This means that a mere 10 percent of the population 60 years and over in the country have protection against the seasonal flu strain at the time they had the vaccine.
In the same vein, only 53% of those who are aware of the pneumococcal vaccine said that they have been vaccinated with it. While the level is a bit higher than flu vaccine coverage, this only translates to a fifth of all Filipinos 60 and over that have protection against pneumonia at least in the next five years after vaccination (Figure 2).
For both vaccines, about 19 percent of Filipinos 60 and over are aware but are not vaccinated for either one of them. This group is characterized as belonging to the older age groups, males, rural residents, poor, and less educated.
Medical experts confirm the underuse of adult immunization in the country, a trend that is consistent with global pattern but more so in areas where other health priorities of treatment rather than prevention dictate use of limited resources (Berba, 2006). Immunization for older persons has not reached the mainstream practice of primary care physicians who take care of the majority of OP (Ramos, M., personal communication. 9 April 2021). Indeed, immunization for older Filipinos has not received much needed attention from among physicians, policy makers and the OP themselves.
What do low levels of vaccine awareness and coverage mean in protecting older people against COVID 19?
A significant finding of the LSAHP is the low level of awareness among older people of vaccines that are available for them. The flu and pneumococcal vaccines have been part of the government health programs for senior citizens since 2011 (A. O. 2011-0018). The fact that only a third are aware of flu vaccines and 41 percent of pneumococcal vaccines in 2018 reflect the failure to reach and inform this segment of the population of important public health programs. Consequently, despite awareness of vaccine availability, only a minority of older people were vaccinated with either flu or pneumococcal vaccines.
The WHO (2019) listed vaccine hesitancy as one of the top ten global health threats. Vaccine hesitancy refers to “the delay in acceptance or refusal of vaccines despite availability of vaccine services” (World Health Organization [WHO], 2015). Its level, determinants, and consequences are complex and context-specific, and may vary across time, place, and vaccines (WHO, 2015).
One year into the COVID-19 pandemic, the Philippines has yet to contain the spread of the virus with alarming resurgence of caseload reported in recent days.2 While it is safe to assume that awareness about vaccine is high across all age groups now, the disproportionate share of OP among the COVID-19 deaths requires an acceleration of the vaccination effort particularly for this age group given earlier analysis which showed 58 percent of older Filipinos have at least one of the risky co-morbidities for COVID-19 (UPPI and DRDF, 2020a). Our study findings also identified groups of older people who displayed possible hesitancy to avail of vaccines: older age group, males, disadvantaged in terms of education and economic status and rural residents.
Based on the DOH COVID Vaccine Sectoral Survey report released recently, there is some hesitancy among OP towards the COVID-19 vaccine (DOH, 2021c). In a sample survey of 812 senior citizen respondents conducted for the period December 2020 to January 2021 among OP ages 60-94 with representation from all regions of the country, results show a moderate trust (47%) on COVID-19 vaccine if it were made available to them. At least 28% said they have very little or no trust at all, exceeding the proportion who signified higher than moderate trust (25%). This low trust in vaccination is surprising given the high proportion (72%) of them who think that the COVID-19 vaccine is very important for their health. Despite the less-than-ideal level of trust on COVID-19 vaccine, 58% are willing to be vaccinated if a vaccine is available while 62% are very willing to be vaccinated if the vaccine is ‘free, deemed safe, effective and approved for use’.
Previous public health crises particularly the controversies surrounding Dengvaxia3, may have affected the population’s confidence in the government’s vaccination program. With low levels of immunization among older persons to start with, such controversy has put the vaccination programs in question (DOH, 2019; WHO, 2019). Vaccine coverage for infectious diseases affecting children, such as tuberculosis, poliomyelitis, diptheria, tetanus, pertussis, and measles declined significantly from 2010 to 2015 (Reyes, et. al. 2020).
The unprecedented economic and social consequences of the COVID-19 pandemic, coupled with the awareness of the steeper risks of infection and mortality among those in the advanced ages, will hope to encourage OP to cooperate in the ongoing vaccination program. To do this however will require a restoration of public trust in the government’s vaccination program not to mention an unhampered supply of vaccines of choice. Reports show that as of the end of March 2021, the national government has not yet signed a single contract to purchase a single dose of Western vaccine and only Chinese vaccines have been procured by the government so far (Carpio, 2021). Confidence-building on vaccines will rely on a system built on credibility, non-partisanship, transparency, public participation, and equity (Lasco and Yu, 2021). Failure to do so will drag the effort to contain the infection and mortality rates from COVID-19 for the country in general and the vulnerable older Filipinos in particular.
References:
Berba, R.P. (2006). Is it Worth it to bring in lolo & lola for a second round of bakuna?, In S.F. de Vega (Ed.). Maximizing the quality of life of the elderly through better health (pp. 21-30). National Academy of Science and Technology, Philippines
Carpio, A.T. (2021, April 1). Where are the vaccines? Crosscurrents article, Philippine Daily Inquirer. https://opinion.inquirer.net/138990/where-are-the-vaccines
Cepeda, M. (2018, February 2). 3 out of 14 kids died of dengue fever after Dengvaxia shot—UP-PGH panel. Rappler. https://www.rappler.com/nation/children-dead-dengue-dengvaxia-up-pgh-panel
Cheng, K.J.G., Rivera, A.S., Lam, H.Y., Ulitin, A.R., Nealon, J. Dizon, R., and Wu, D. (2020). Influenza-associated excess mortality in the Philippines 2006-2015. PlosOne. 15(6). Doi:10.137i/journal.pone.0234715.
Department of Health. (2021a, April 2). DOH COVID-19 Case Bulletin #384.
Department of Health. (2021b, April 3). DOH COVID-19 Case Bulletin #385.
Department of Health. (2021c). Dissemination of the Results of COVID Vaccine Sectoral Survey Round 1 to DOH Central Office (Department Memorandum No. 2021-0090).
Department of Health. (2019). DOH expands measles outbreak declaration to other regions. https://doh.gov.ph/node/16647
Department of Health. (2011). Implementing Guidelines on Influenza and Pneumococcal Immunization for Indigent Senior Citizens (Administrative Order No. 2011-0018).
Department of Health. (2015). National Policy on the Health and Wellness Program for Senior Citizens (Administrative Order No. 2015-0009).
Heo, J. Y., Song, J. Y., Noh, J. Y., Choi, M. J., Yoon, J. G., Lee, S. N., … & Kim, W. J. (2018). Effects of influenza immunization on pneumonia in the elderly. Human vaccines & immunotherapeutics, 14(3), 744-749.
Kostova, D., Reed, C., Finelli, L., Cheng, P. Y., Gargiullo, P. M., Shay, D. K., … & Bresee, J. S. (2013). Influenza illness and hospitalizations averted by influenza vaccination in the United States, 2005–2011. PloS one, 8(6), e66312.
Lasco, G., and Yu, V. G. (2021). Communicating COVID-19 vaccines: Lessons from the dengue vaccine controversy in the Philippines [Commentary]. BMJ Global Health, 6: e005422. doi:10.1136/bmjgh-2021-005422
Reyes, M.S.G., Dee, E.C., and Ho, B.L. (2020). Vaccination in the Philippines: experiences from history and lessons for the future. Human Vaccines and Immunotherapeutics. In https://doi.org/10.1080/21645515.2020.1841541
Smetana, J., Chlibek, R., Shaw, J., Splino, M., & Prymula, R. (2018). Influenza vaccination in the elderly. Human vaccines & immunotherapeutics, 14(3), 540-549.
University of the Philippines Population Institute (UPPI) and Demographic Research and Development Foundation, Inc. (DRDF). (2020a, March). COVID-19 and the Older Filipino Population: How Many Are at Risk? (UPPI/DRDF Research Brief No. 1). https://www.uppi.upd.edu.ph/sites/default/files/pdf/COVID-19-Research-Br….
World Health Organization. (2019, February 13). Immunization gaps contribute to rising measles cases in the Philippines. https://www.who.int/philippines/news/feature-stories/detail/immunization…
World Health Organization. (2015, August 18). Vaccine hesitancy: A growing challenge for immunization programmes. https://www.who.int/news/item/18-08-2015-vaccine-hesitancy-a-growing-cha…
1 LSAHP is the first nationally representative longitudinal study on aging and health in the Philippines conducted by the Demographic Research and Development Foundation, Inc. with funding from the Economic Research Institute for ASEAN and East Asia. The 2018 LSAHP report may be accessed at https://bit.ly/drdf-aginghealthph
2 DOH recorded 15,310 new confirmed COVID-19 cases on April 2, 2021 (DOH, 2021a), the highest single-day tally since the start of the pandemic in the country. However, considering the 3709 case backlogs noted by the department on April 2 due to some technical issues, the highest single-day tally of confirmed infection is on April 3 with 12,576 new cases (DOH, 2021b).
3 In 2017, Dengvaxia, the first commercially approved dengue vaccine developed by Sanofi, was administered to over 800,000 public school children through a mass vaccination program and allegedly led to 14 deaths. However, an investigation conducted by a panel of medical experts concluded that only three of these 14 deaths were associated with the vaccine; that is, the children developed dengue fever despite being vaccinated and died due to the disease (Cepeda, 2018).
This research brief was prepared by Grace T. Cruz, Elma P. Laguna, Mark Ryan B. Paguirigan, Maria Karlene Shawn I. Cabaraban, Maria Midea M. Kabamalan, Maria Paz N. Marquez, and Christian Joy P. Cruz.
Suggested citation: University of the Philippines Population Institute (UPPI) and Demographic Research and Development Foundation, Inc. (DRDF). (2021, April). Vaccinating the most vulnerable group in the time of pandemic: Insights from a national survey of older people (UPPI/DRDF Research Brief No. 9). Retrieved from https://www.uppi.upd.edu.ph/sites/default/files/pdf/COVID-19-Research-Brief-09.pdf.
