
The changing demographics of COVID-19 infections and deaths in the Philippines: how age-sex structure, living arrangement, and family ties intersect
The University of the Philippines Population Institute (UPPI) in collaboration with the Demographic Research and Development Foundation (DRDF) are sharing results of their demographic studies to provide the Philippine context on the possible effects of the coronavirus disease (COVID-19) pandemic. In both the UPPI and DRDF websites, we are publishing a series of research briefs focusing on various aspects of Filipino lives that are affected by COVID-19, in both the short and long terms.
Download PDF here.
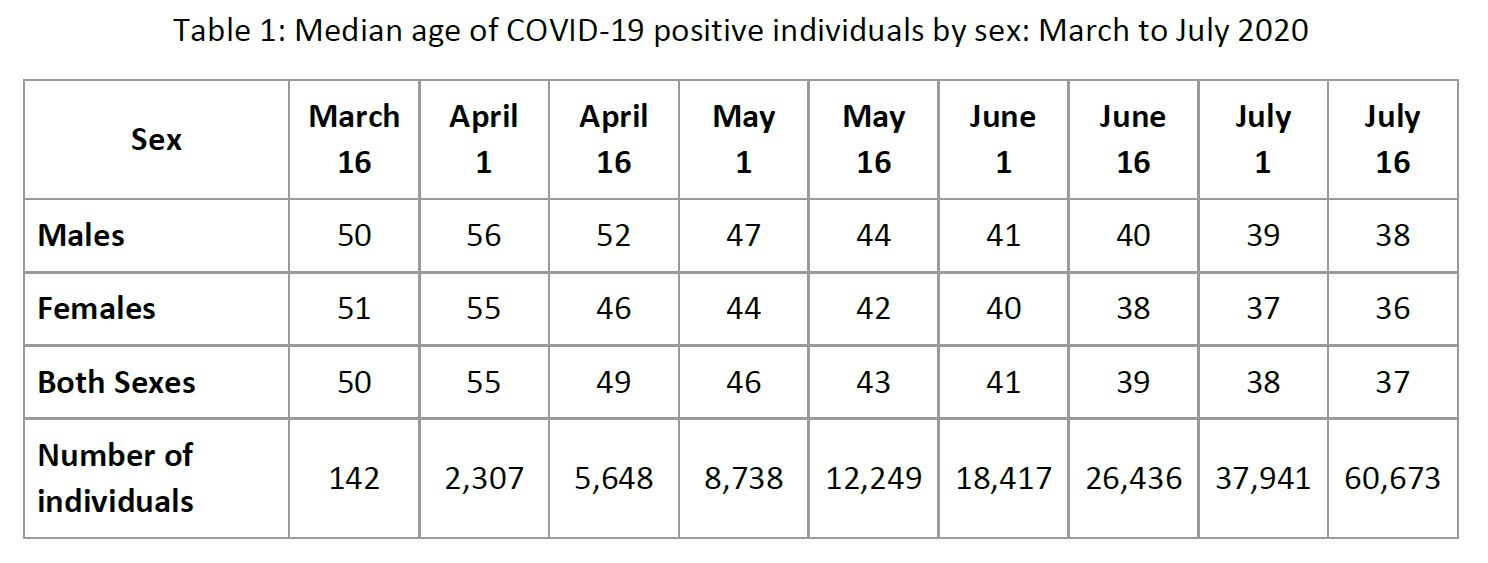
When community transmission of COVID-19 became apparent in the Philippines, older persons were deemed most vulnerable mainly because they tend to have comorbidities that make them at higher risk to COVID-19 infection (see UPPI and DRDF, March 2020, Research Brief 1). Around the time the National Capital Region (NCR) was placed under enhanced community quarantine (ECQ) (16 March 2020), there were already 142 COVID-19 positive cases all over the country based on the data provided publicly by the Department of Health (DOH). These infected individuals have a median age of 50 with women slightly older than men (51 vs 50 years) (Table 1).
Over time and as the number of cases increased, the distribution across age groups has shifted, skewing towards the younger population. In mid-July 2020 or 4 months after various levels of community quarantine were imposed, the median age of COVID-19 positive individuals has declined to 37 years old. By then, COVID-19 positive women are found to be two years younger on average than men, in contrast to the pattern found four months earlier.
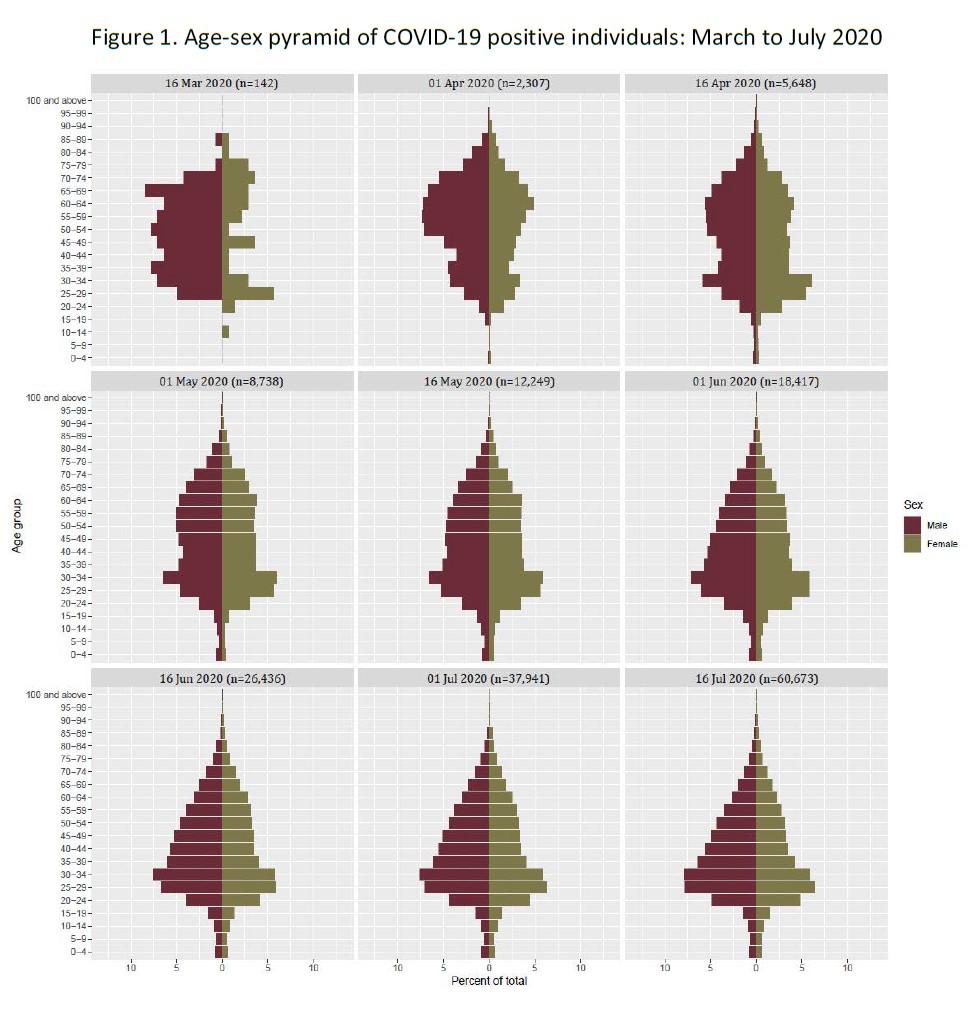
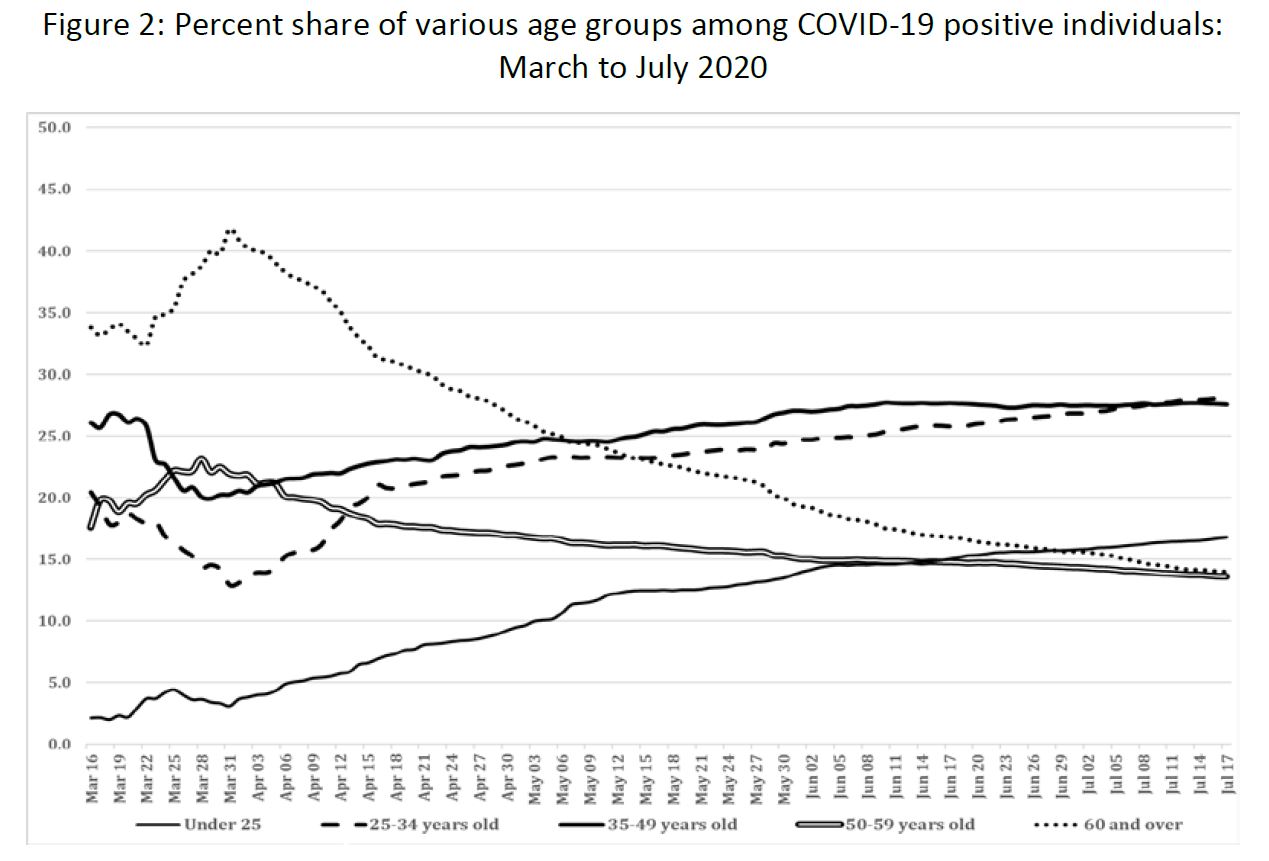
The set of age-sex pyramids shown in Figure 1 depicts the changing age distribution of male and female individuals who tested positive from COVID-19 from 16 March to 16 July 2020. What is noteworthy is the shift in the infections to the younger ages with observable increasing share of individuals in the age group 25-34. At the start of the community quarantine in mid-March 2020, this age group accounted for 20% of cases (Figure 2). The share dropped to 13% two weeks after, but thereafter had continuously increased and reached 28% by 16 July. Similarly, an increasing pattern is also found in the younger age groups (below age 25), and those 35-49 years old while the share of COVID-19 positive individuals in the older ages of 50-59 and 60 and over declined.
What changing age demographics have to do with COVID-19 deaths?
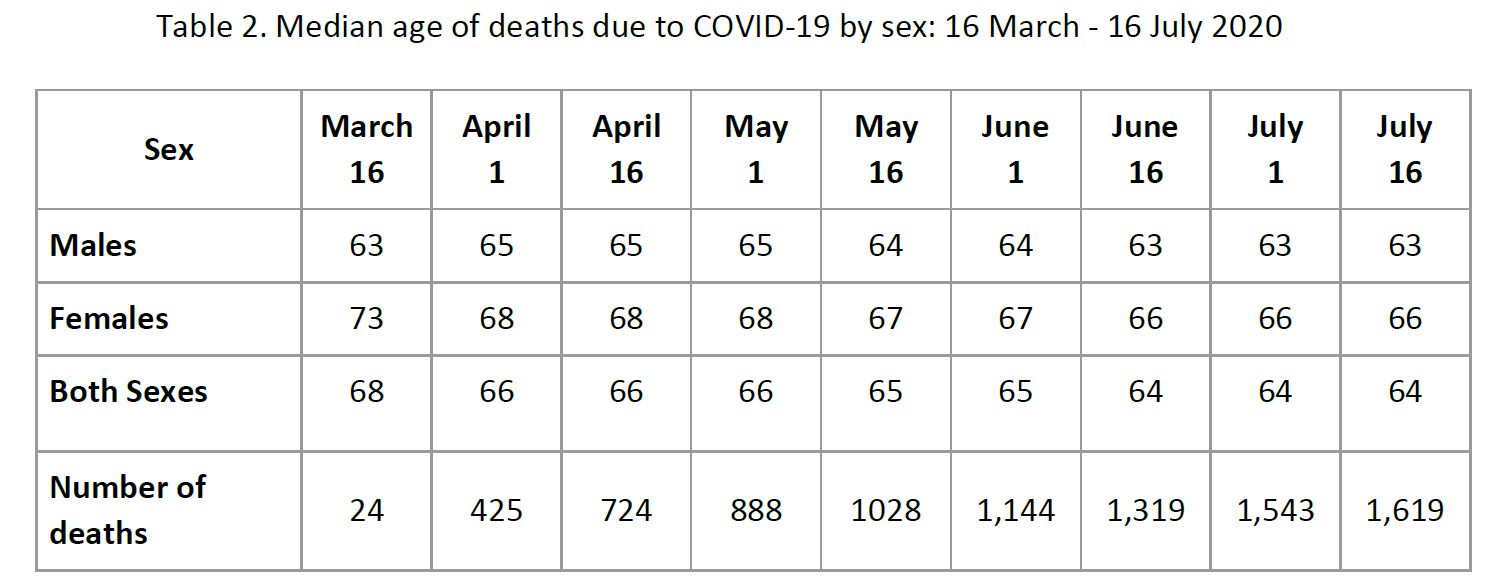
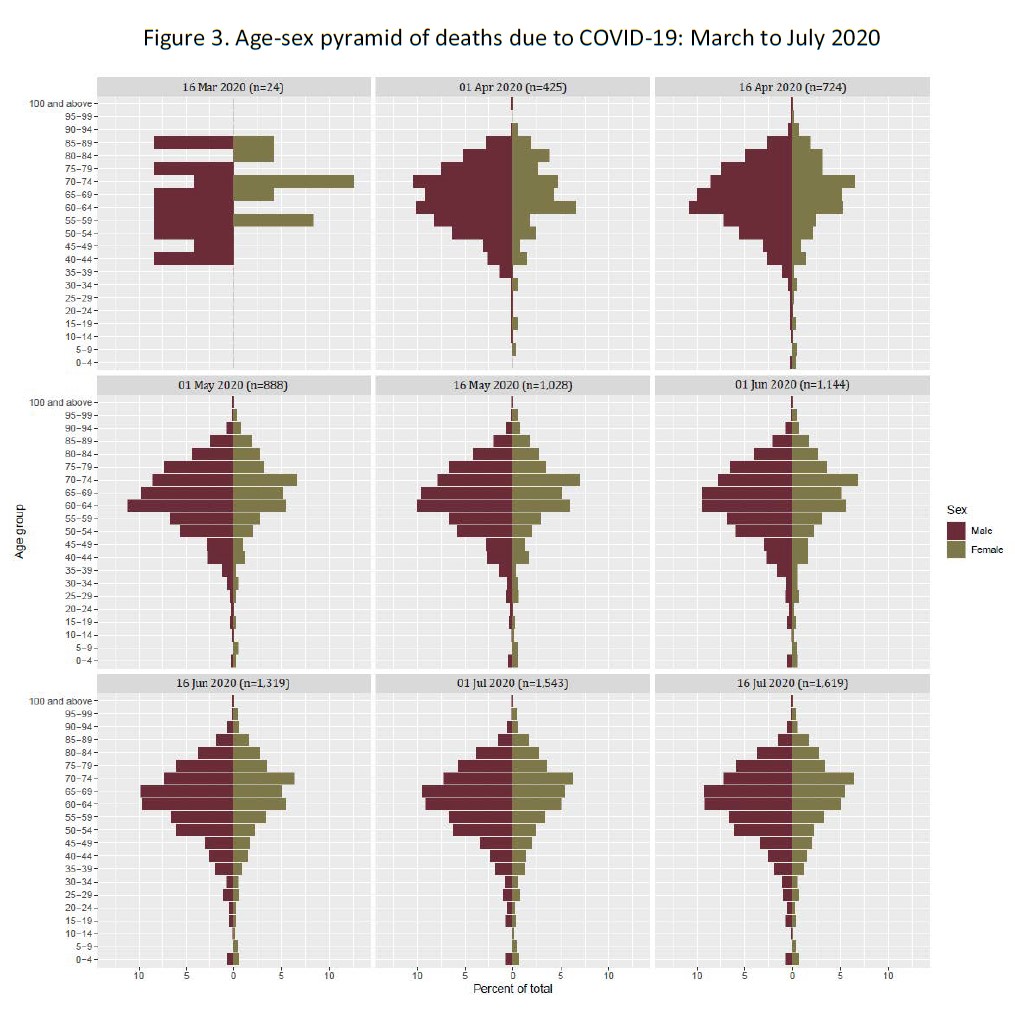
The shift in the distribution of COVID-19 positive individuals to younger age groups has consequently led to a slight expansion of COVID-19 deaths to younger population. In 16 March, with 24 recorded deaths, all are above age 40. By 16 July when death toll reached 1,619, all age groups have recorded deaths. Similarly, the median age of those who died from COVID-19 declined, from 68 years in 16 March to 64 by 16 July 2020 (Table 2). Men who succumb to COVID-19 are also generally younger than women.
COVID-19 deaths show a lopsided sex distribution with twice as many men than women deaths noted in the early part of the pandemic (Figure 3). As the pattern starts to stabilize, the sex ratio of deaths shows a declining level registering 163 male deaths per 100 female deaths as of 16 July 2020.
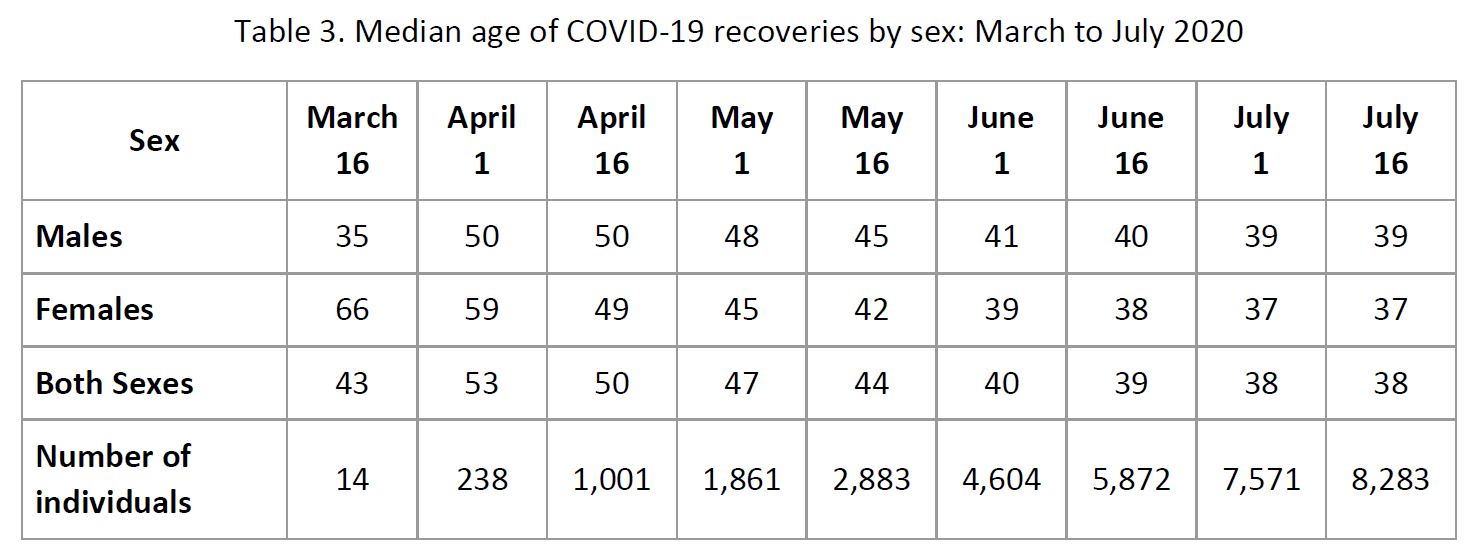
Consistent with the shifting trend towards the younger population of infections and mortality due to COVID-19 is a similar trend in COVID-19 recovery. Data show that the median age of recovery declined by 5 years within the four months observation period, from 43 to 38 years (Table 3). Except for the very small number of recoveries reported in 16 March, the declining age of recovery is observed for both men and women as indicated by the monotonic decrease in age over time.
What accounts for the shift in age distribution of COVID-19 infections and deaths?
Early studies on COVID-19 (see Dowd, et. al., 2020; Esteve, et. al, 2020) have shown that the variation in infections and deaths across countries may be explained by the population age structure. Countries characterized as “ageing”, or where the proportion of older persons aged 60 and over have reached at least 10% of the population are expected to have higher infection rate and case fatality rate among older age groups. While only eight percent of the Philippine population are in the age group 60 and over, they account for majority of all COVID-19 deaths so far. And while individuals below age 60 dominate the COVID-19 positive cases, they account for only a third of total deaths.
In addition to age structure, studies from Italy and Spain (Dowd, et. al., 2020; Esteve, et. al., 2020; Mogi and Spijker, 2020) noted the importance of understanding how different age groups interact in societies as manifested in living arrangement, age composition of households and intergenerational contacts. The spread of COVID-19 in Italy, for instance, was attributed to higher intergenerational contacts as younger family members tend to commute from cities to the villages to visit their parents and grandparents (Dowd, et. al., 2020; Rotondi, et. al., 2020).
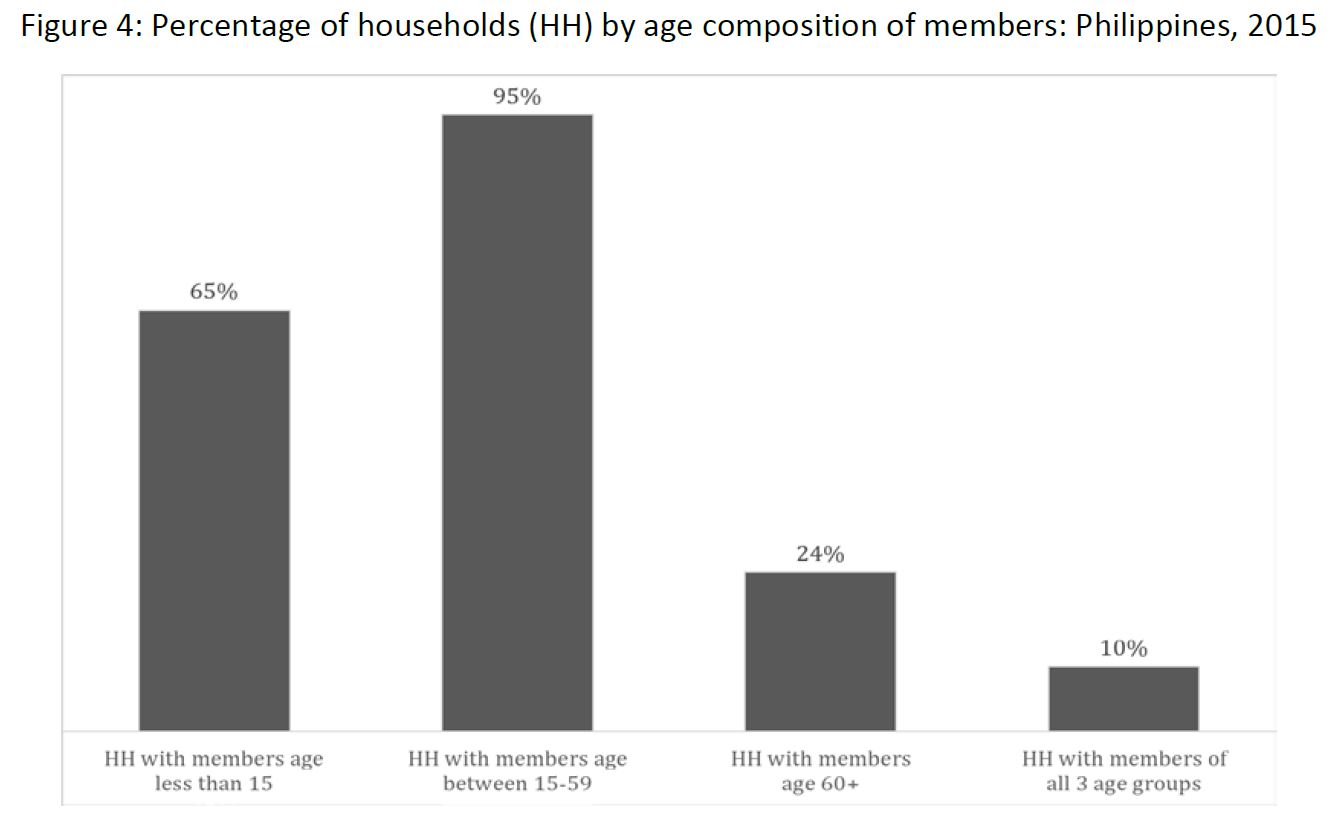
Based on the 2015 Census of Population and Housing, the average household size in the Philippines is 4.4. In terms of age structure, an overwhelming majority (95%) of Filipino households have members in the working age group, 15-59 years (Figure 4). Sixty five percent have members who are aged below 15 years while almost a quarter have members who are 60 years old and over. Ten percent of households are composed of members from the three age groups: young (below 15 years), working age (15-59) and old (60 and over). Moreover, co-residential living arrangement is common among Filipino families. In the study of older Filipinos 60 years old and over conducted in 2018, only 13% reported that they live alone; majority are living with at least one adult child (Cruz, et. al., 2019).
Meanwhile, for the period May to July 2020, a noticeable spike in the number of COVID-19 infections is found in the age group 25-34. This is a working age population and they are likely more mobile compared to other segments of the population. As the level of community quarantine is lowered and restrictions are eased, the mobility of those in the working age group has also likely increased. This may become a cause for concern because COVID-19 transmission in younger age groups may go undetected for a longer period because they are also less likely to have co-existing health conditions and may be asymptomatic. Based on DOH COVID-19 Data Drop of 17 July 2020, a third of asymptomatic cases are found in the age group 25-34 and about one-fourth are less than 25 years old.
Does the restriction on movement of older persons protect them from COVID-19 infection?
As the total number of COVID-19 cases continued to increase in the country, there is an observed surge of infection among the younger age groups. And while the relative share of the older age groups started to decline, their absolute number steadily increased over time. Limiting movement of older people does not protect them completely because they are still exposed to possible carriers such as their younger household members. Moreover, as the government eased the restrictions on the movement of older people following the negative reactions on the directive on their confinement, older people started to resume their work and other activities outside their homes making them more exposed to possible infection. Based on the 2015 Census of Population and Housing, approximately eight percent of gainful workers are older persons ages 60 and over.
Discussion and ways forward
The demographic trend in COVID-19 infection, death and recovery in the Philippines is changing. Early data show the vulnerability of the older people as shown by their significant share of COVID-19 infections and deaths. Four months since the onset of community transmission, as well as the imposition of different levels of community quarantine and measures such as physical distancing and observance of proper hygiene, COVID-19 infections in the country continue to spread and increase. More recent data indicate a shifting pattern skewing towards the younger age groups.
The shift in the age distribution of COVID-19 infection identifies critical age groups: the working age population, particularly those in ages 25-34 and 35-49. The spike of cases in these age groups happened when restriction on movement was lifted and when more people were allowed to return to work. It is imperative therefore that workers should be tested for COVID-19 before they will be allowed to report for work. Companies should ensure close monitoring of its employees through regular testing and possibly explore the use of monitoring apps to track the health status and risk of COVID-19 infection among their employees.
Filipino families are often characterized by its strong family ties and coresidential arrangements. Filial norms, intergenerational relationships and family support are considered important values instilled among family members that serve as safety nets particularly for the vulnerable groups. However, a pandemic such as COVID-19 puts into question whether our valued norm of strong family ties and relationship as manifested in multigenerational living arrangement and strong intergenerational contacts present potential threat.
The strategies imposed by the government to contain the spread of COVID-19 entail great sacrifice to everyone. The community quarantine found families, in some instances, several generations, young and old, being cooped up together in congested environment which presents greater risks of viral transmission. Families will have to take it upon themselves to observe physical distancing, wash hands, wear mask, limit mobility, and observe protocol when going out and coming back to their homes in order to protect one another in the household. While face to face interaction may be limited, caring for each other can still be manifested in other forms.
Notes on the COVID-19 data:
This research brief uses the 17 July Data Drop from the Department of Health (DOH). Only those with information on age, sex, and dates (of reporting, of recovery, and of death, as applicable) were included in the analysis.
Of the 63,001 COVID-19 cases in the Data Drop, there are 494 cases without information about age. These were excluded from the analysis and did not affect the age distribution of cases.
Similarly, out of the 1,660 deaths reported as of 17 July, there are 39 cases excluded from the analysis because they have no information on date of death, and an additional 2 cases were excluded because they have no information about age.
Finally, while there is a total of 21,748 recoveries on record as of 17 July, only 8,302 have information on date of recovery. An additional 19 cases were excluded because they did not have information on age, leaving 8,283 cases (38% of reported recoveries) for analysis.
References:
Cruz, G.T., Cruz, C.J.P. & Saito, Y. (eds.) (2019). Ageing and Health in the Philippines. Jakarta: Economic Research Institute for ASEAN and East Asia (ERIA).
Dowd, J. B., Andriano, L., Brazel, D.M., Rotondi, V., Block, P., Ding, X., Liu, Y. & Mills, M.C. (2020). Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences, Apr 2020, 202004911; DOI: 10.1073/pnas.2004911117
Esteve, A., Permenyaker, I., Boertien, D., Vaupel, J. 2020 National age and co-residence patterns shape COVID-19 vulnerability. MedRxiv. doi:110.110112020.05.13.20100289.
Mogi, R. & Spijker, J. (2020). The influence of social and economic ties to the spread of COVID-19 in Europe. SocArXiv, April 14. doi:10.31235/osf.io/sb8xn.
Rotondi, V., Andriano, L., Downd, J. B. & Mills, M. C. (2020). Early evidence that social distancing and public health interventions flatten the COVID-19 curve in Italy. OSF Preprints, April 26. doi:10.31219/osf.io/wah4e.
This research brief was prepared by Maria Midea M. Kabamalan, Elma P. Laguna, Klarriness P. Tanalgo, Grace T. Cruz, Maria Paz N. Marquez.
Suggested citation: University of the Philippines Population Institute (UPPI) and Demographic Research and Development Foundation, Inc. (DRDF). (2020, July). The changing demographics of COVID-19 infections and deaths in the Philippines: how age-sex structure, living arrangement, and family ties intersect (UPPI/DRDF Research Brief No. 7). Retrieved from https://www.uppi.upd.edu.ph/sites/default/files/pdf/COVID-19-Research-Brief-07.pdf.
